
On Monday through Thursday mornings, Rodolfo “Rolo” Lopez Jr. and Angel Ojeda, research assistants and certified phlebotomists in Internal Medicine, head to work at 270 Congress Avenue, the “storefront” for Yale Clinical and Community Research, to stock the Community Health Care Van (CHCV). The doors bang open on the 40-foot-long blue vehicle as they add what they need for the day: sterile syringes, medical supplies, and naloxone, a medicine used to reverse an opioid overdose.
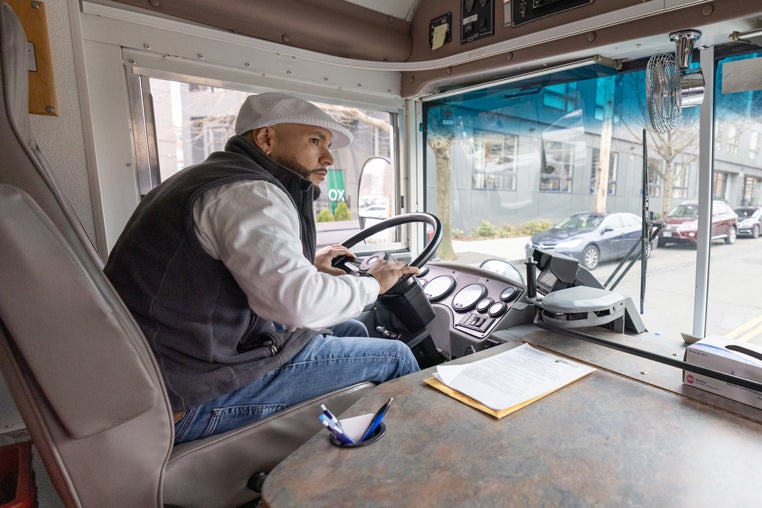
 Rolo Lopez Jr. stocks a smaller van that he occasionally uses to run the Syringe Services program in New Haven communities.
Rolo Lopez Jr. stocks a smaller van that he occasionally uses to run the Syringe Services program in New Haven communities.
Joining them is the CHCV’s clinical director, Deirdre Gruber, APRN. She is always on board to provide primary-care services as the trio sets off to New Haven’s high-risk areas— currently including Fair Haven, the Hill, Dixwell Avenue, and the New Haven Green—to provide harm reduction services through free care that centers on the needs of people who use drugs, not on the stigma of drug use. It is the first such program in the country and has continuously operated since 1993. Harm reduction aims to lessen the harmful effects of drug use, including transmission of infectious diseases and overdose. The neighborhoods the van frequents are known areas easily accessible for people who use drugs, engage in sex work, and people with unstable housing. Once Lopez and Ojeda park the van in a designated area, usually from 9:00 a.m. to noon, it transforms into an instant and comprehensive mobile clinic.
“We’ve had such a presence in the community for so long that a lot of people know who we are and what we’re providing,” said Ojeda. “When we test people and they are positive for STIs, Hep C virus (HCV), or HIV, we offer treatment, link them to care, connect them to case managers, and help with homelessness. When they test negative for HIV and want to remain negative, we offer them PrEP, a drug regimen called Pre-Exposure Prophylaxis, or PEP, Post-Exposure Prophylaxis.”
“It is a busy van experience,” added Gruber, who joined Yale five months ago after spending her career in public health, including a stint at the New Haven Health Department. “My job is to respond to patients’ medical needs—checking their blood pressure or refilling their hypertension medication—and if they present with extenuating medical problems, to triage, treat, and coordinate care as needed.” Linking patients to care often means connecting them to Yale research studies where researchers can help them get into treatment, and sometimes even into housing.
 Deirdre Gruber, APRN, CHCV’s clinical director, provides primary care services on the van.
Deirdre Gruber, APRN, CHCV’s clinical director, provides primary care services on the van.
Lopez noted that their handling of medical case management for people with HIV includes conducting re-entry case management for people released from incarceration. They will see clients a couple of months before their release and assist them with medical and mental health care, housing, and insurance when they are out of prison.
“We have our needle exchange program for people who inject drugs,” said Lopez. “When they’re ready to get clean, we help them enter drug-treatment programs and get access to methadone or suboxone prescriptions, whichever one works best for the client. We do a lot for the undocumented and uninsured population. We can draw blood for people who want to get tested for HIV, Hepatitis, and STIs for free. And if the results come back positive, we can provide treatment and linkage to free care programs.”
An oasis in a care desert
Rick Altice, professor of medicine (Infectious Diseases) and of epidemiology (Microbial Diseases), is the founder of the CHCV, which is entirely grant-funded. The CHCV emerged from the pilot study of the first syringe services program (SSP) in the country that was evaluated from 1989 through 1992 to prevent HIV transmission where many people who injected drugs were marginalized from healthcare. The first CHCV in 1993 involved a small Winnebago that Altice drove himself, along with a volunteer social worker and a licensed HIV counselor, to meet the needs in New Haven’s most marginalized neighborhoods.
 Rick Altice, founder of the CHCV, and Rodolfo “Rolo” Lopez Sr. (Photo provided by Rick Altice).
Rick Altice, founder of the CHCV, and Rodolfo “Rolo” Lopez Sr. (Photo provided by Rick Altice).
“Our surveys indicated that our SSP clients had minimal access to community care, including for infectious diseases like HIV, HCV, or TB, paving the way for us to tailor services for our clientele,” said Altice. “We primarily served people with substance use disorders, a concept that was not easily accepted by the traditional healthcare settings or even the community, as there was considerable resistance to supporting our clients. Such factors undermined our ability to generate sufficient funding to support the community. Our services grew over time. We were the first to prescribe buprenorphine from a mobile medical clinic, often eclipsing treatment in other settings, and the first to support adherence to complex medication regimens by supervising medication-taking. For those who sought addiction treatment outside our program, we provided free physical exams to increase access to restrictive services. As such, we re-engineered how care was delivered.”
Over time, published research studies confirmed the benefits between mobile medical clinics and better health outcomes. In the case of HCV infections, when new, easier to tolerate, and effective medications were approved by the FDA, these treatments were made available at the storefront on Congress Avenue and on the CHCV. By 2017, the City of New Haven recognized that the CHCV and storefront were making enough of an impact on the community that it transferred the syringe-services program to them so that an integrated service delivery program aligned health and prevention needs.
 The CHCV emerged from the pilot study of the first syringe services program (SSP) in the country that was evaluated from 1989 through 1992 to prevent HIV transmission where many people who injected drugs were marginalized from healthcare. (Photo provided by Rick Altice).
The CHCV emerged from the pilot study of the first syringe services program (SSP) in the country that was evaluated from 1989 through 1992 to prevent HIV transmission where many people who injected drugs were marginalized from healthcare. (Photo provided by Rick Altice).
“I was always the poor kid known for living in a single-wide trailer without running water in rural Florida. No matter how smart I was or how hard I worked, I was still that kid,” said Altice. “This experience, however, imbued me with a real sense of health and human rights and social justice. I had aligned my mission to be connected to the health of those in low- and middle-income families. The AIDS epidemic, a game-changer for me personally and professionally, led me to work at the CDC as a medical student from 1981 to 1983. As a gay man, I certainly could identify with the people identified as at-risk in an epidemic, but I often viewed people who inject drugs, people deprived of liberty, and sex workers as more marginalized, and aligned myself with addressing health disparities for all people with or at risk for HIV.”
“It’s not our place to judge”
Lopez and Ojeda are lifelong New Haven residents. The people they help are not only neighbors, but sometimes friends and family.
Lopez has been in his position for five years, following in the footsteps of his father, Rodolfo “Rolo” Lopez Sr., who also worked on the CHCV. “My father was in this field at Yale for 20 years and just retired,” said Lopez. “I was always interested in his work, and I grew up in the community we serve. Dad did a lot of case management for people with infectious diseases and was exceptionally compassionate.”
 Angel Ojeda was hired as a driver in 2006 and has been promoted over the years, while taking advantage of professional training. (Photo by Robert DeSanto).
Angel Ojeda was hired as a driver in 2006 and has been promoted over the years, while taking advantage of professional training. (Photo by Robert DeSanto).
LKL Winners two years in a row
In recognition of the community care provided in New Haven by staff at Yale’s Center for Clinical and Community Research, including the Community Health Care Van and the storefront, Rodolfo Lopez Jr., Angel Ojeda, and former colleague Terry Bohonnon received the Linda Lorimer Award for Distinguished Service in 2022. Their citation read, in part, “Throughout the pandemic and beyond, they have unfailingly offered a caring and trusted environment for those in need of addiction services and medical treatment.”
A year later, Natalie Kil was chosen for her work in improving the health of the New Haven community, “partnering with local health services to curb the opioid epidemic and launching groundbreaking harm-reduction programs to prevent the spread of HIV, among other health initiatives.”
Ojeda was hired as a driver in 2006 and has been promoted over the years, while taking advantage of professional training. “When I became a young adult, it felt really good to help people who came from the same background as me,” he said. “Some made it to high school and college, and some fell into the jail system and the drug addiction system.”
“I grew up in one of the high-risk areas here in New Haven, so the people I help are just like me,” adds Lopez. “They’re regular people. They’re just going through tough times, and many have been through traumatic experiences. It’s not our place to judge; it’s to provide a service and meet them where they are.”
Lopez and Ojeda don’t play down how hard their work can be, but they believe they make a difference and are proud to provide services to help their clients and their community.
“A hard day for me is when I’ve been working for months to build up to a particular housing appointment to help a client get housing, and they miss it because they’re too intoxicated or just not ready to go,” said Lopez. “It’s frustrating because I feel so bad for the clients. I’ve built a bond and want to help them so much, sometimes more than they want to help themselves at that moment.”
“When I lose a client when he or she dies on me, I think that’s one of the hardest things to deal with,” said Ojeda. “I’ve lost two of them, and it’s like losing a family member. Addiction is a rollercoaster, and some people don’t believe that relapsing is part of addiction.”
 Over time, published research studies confirmed the benefits between mobile medical clinics and better health outcomes. (Photo by Robert DeSanto).
Over time, published research studies confirmed the benefits between mobile medical clinics and better health outcomes. (Photo by Robert DeSanto).
Ojeda noted that there are successes, too, and many of CHCV’s clients work hard daily to maintain their success. “Whether a client has relapsed two or 27 times, there’s always that one time when they stay sober longer and longer,” he said. “They get their kids back. They get housing; some of them even get jobs or want to work in our field. They’re pulling up in cars. They look great, and they never go back to addiction, but you know they fight it every day.”
Storefront Samaritans
Lopez and Ojeda begin and end their workday at the storefront at 270 Congress Avenue. Under the direction of Altice, it has been a trusted environment for those needing treatment and prevention for addiction and medical care since 1993 and home to New Haven’s SSP, the largest in Connecticut, since 2017. The staff of 14 includes Gruber, Natalie Kil, associate director for domestic projects, and Orawan Gardner, a psychiatric nurse practitioner.
While Lopez and Ojeda provide community care on the mobile clinic, the storefront’s doors are open all day. Gruber, Kil, and their colleagues provide harm-reduction for walk-ins, administering primary-care services, addiction treatment services, performing street-drug testing and rapid testing for Hepatitis C and HIV, and offering treatment. Patients can also refill prescriptions.
 Natalie Kil, associate director for domestic projects, in conversation with Orawan Gardner, a psychiatric nurse practitioner. (Photo by Robert DeSanto).
Natalie Kil, associate director for domestic projects, in conversation with Orawan Gardner, a psychiatric nurse practitioner. (Photo by Robert DeSanto).
“Everyone here jumps in to help, and everyone works hard,” said Kil. “We’re serving a group of people who have had terrible experiences almost everywhere they go because they use drugs or lack housing. We provide a little bit of dignity and non-judgment, even for a small part of their day, even though a lot of them are going right back out onto the streets. If we can give them a warm place to charge their phone, if they have one, or a snack or something else, that is what we are here for. Many of them do say, ‘Oh, you’re so nice to us here.’”
House calls help
Pediatric Nurse Practitioner Liz Znamierowski runs the Mother and Infant Mobile Clinic based out of the storefront at 270 Congress Avenue. Launched by Dr. Leslie Sude in 2020, the Mother and Infant program brought care to mothers and newborns in New Haven during the COVID-19 pandemic and revealed that there was enough community need to continue its services beyond the pandemic. In partnership with American Medical Response, the Mother and Infant Mobile Clinic utilizes a retrofitted ambulance to provide dyadic healthcare curbside to patients’ residences.
“For many families, transportation, work, and childcare present a real barrier to attending clinic-based visits. The idea of the mom and baby van is to bring newborn evaluations and maternal health screenings directly to the families,” said Znamierowski.
Mothers are offered lactation support, and families receive information and navigation to community services and timely linkage to adult and pediatric health services. Integral to the Mother and Infant Mobile Clinic services is the identification and prompt referral to escalated care for pregnancy related hypertension, pre-eclampsia, depression, abnormal bleeding, and mental health concerns. The Mother and Infant Mobile Clinic has sparked awareness and conversation locally and regionally, highlighting the value of mobile outreach and the value added to healthcare encounters centered on the mother infant dyad. The current grant funding allows the van to run one day a week, but the hope for more funding is always there.






